Indirect Ophthalmoscopy?
In this blog, we will explore the concept of indirect ophthalmoscopy. But before exploring that, it’s important to understand the nature of ophthalmoscopy.
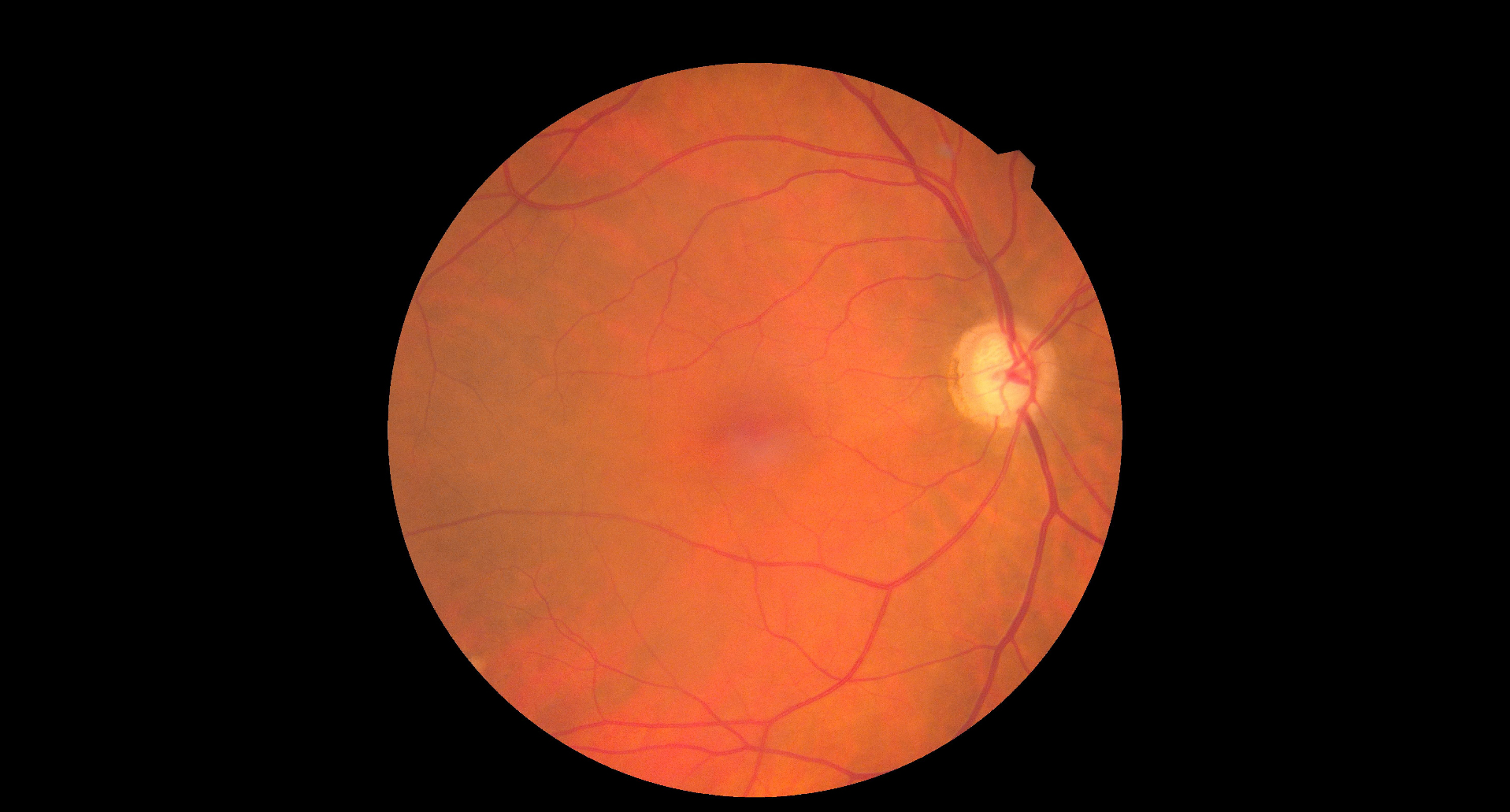
Ophthalmoscopy is a medical examination technique used to view the internal structures of the eye, particularly the retina, optic nerve, and blood vessels. The procedure involves using an instrument called an ophthalmoscope, which illuminates the inside of the eye and magnifies the view for the examiner.
What is Ophthalmoscopy Used For?
Ophthalmoscopy is a versatile tool used for both diagnostic and preventive purposes. Here are some of the primary uses:
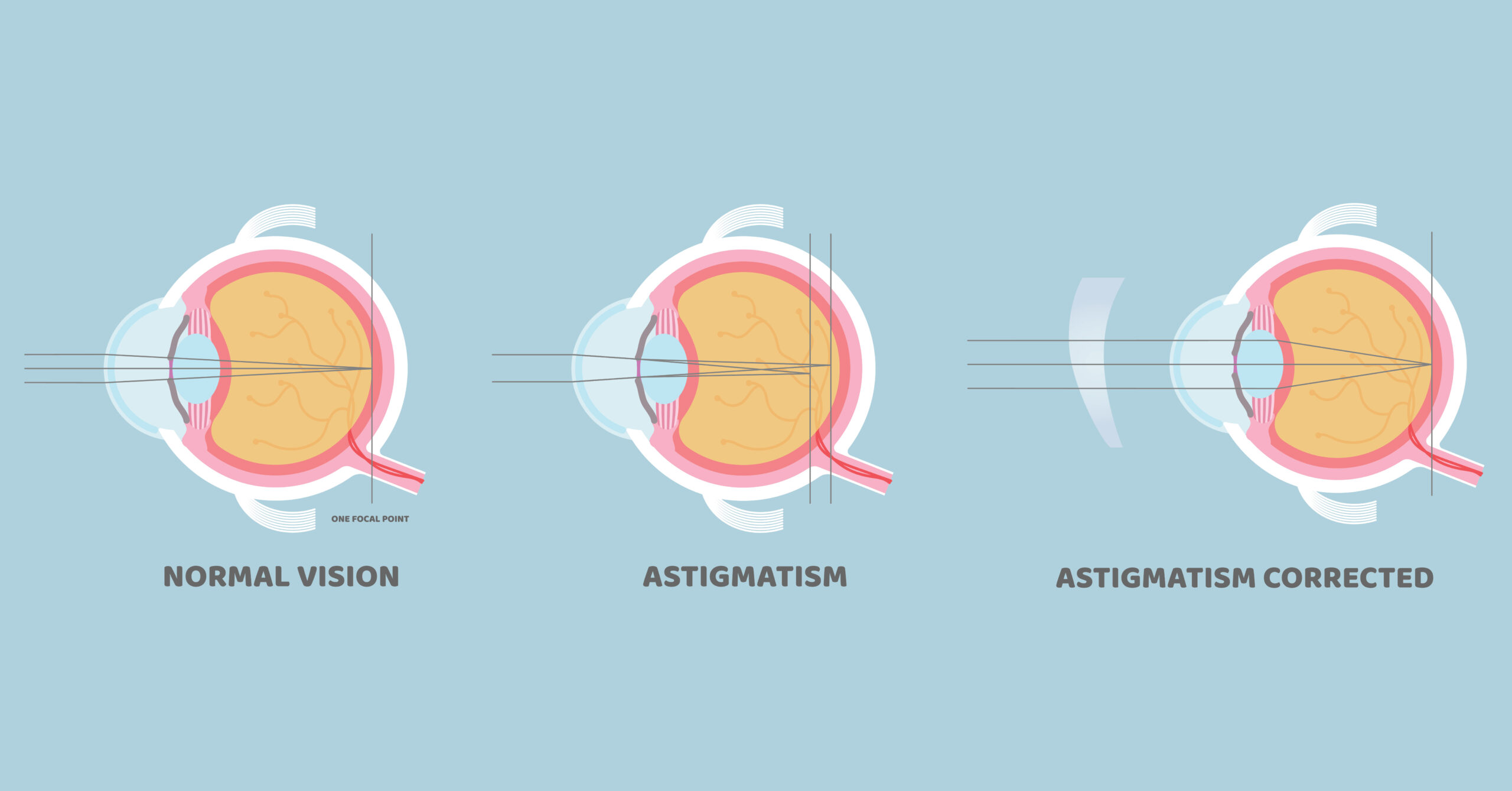
- Diagnosing Retinal Disorders: Ophthalmoscopy helps in the early detection of retinal diseases, such as diabetic retinopathy, macular degeneration, and retinal vein occlusion.
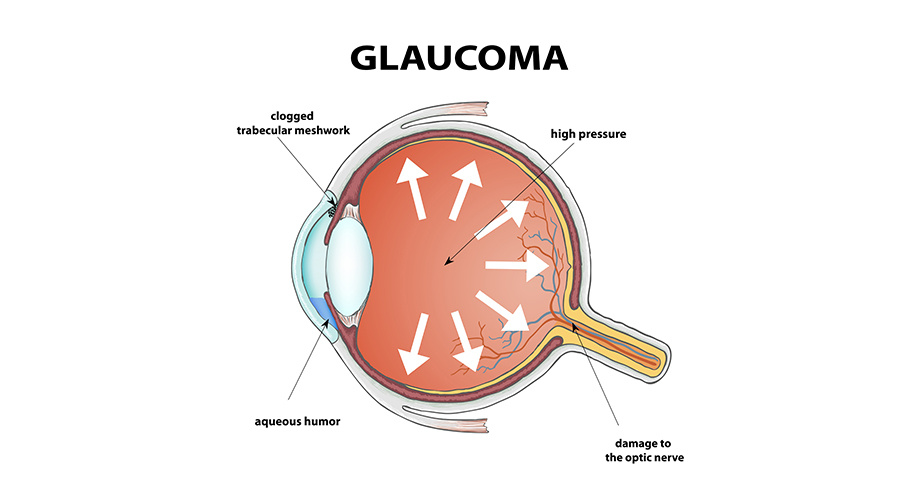
- Monitoring Eye Health: For patients with conditions like glaucoma, ophthalmoscopy can monitor changes to the optic nerve over time. This is crucial in managing disease progression and adjusting treatment plans accordingly.
- Detecting Systemic Conditions: Certain systemic diseases, such as hypertension and diabetes, can affect the blood vessels in the retina. Ophthalmoscopy can help detect early signs of these systemic conditions before they cause more severe damage.
- Assessing the Optic Nerve: Conditions like optic neuritis or increased intraocular pressure can lead to changes in the optic nerve, which can be detected via ophthalmoscopy.
- Evaluating Eye Trauma: Ophthalmoscopy allows the detection of injuries, such as retinal tears, bleeding, or swelling, resulting from trauma to the eye.
There are two primary types of ophthalmoscopy: direct ophthalmoscopy and indirect ophthalmoscopy. Both techniques allow for the examination of the eye’s interior but differ in their approach, equipment, and field of view.
Direct Ophthalmoscopy:
Direct ophthalmoscopy is the more commonly used and simpler form of ophthalmoscopy. It involves the use of a handheld instrument, called a direct ophthalmoscope, which is held close to the patient’s eye. This method provides a magnified view of the retina, but it has a limited field of view. The examiner can examine a small portion of the retina at a time and must move the ophthalmoscope to view different areas. Direct ophthalmoscopy is ideal for quick, focused assessments, and is frequently used during routine eye exams.
Indirect Ophthalmoscopy:
Indirect ophthalmoscopy, on the other hand, is a more advanced technique that offers a wider view of the retina and other parts of the eye. In this method, the examiner wears a specialized headset, which is attached to a light source. A handheld lens is used to magnify the view, allowing the examiner to observe a larger area of the retina at once, including the peripheral regions.
The patient typically needs to lie back in a reclining chair to help position the eye appropriately for the procedure. Indirect ophthalmoscopy provides a three-dimensional view of the retina, making it particularly useful for evaluating retinal conditions like tears, detachments, and diabetic retinopathy. It also allows the examiner to view the optic nerve and macula with greater detail and clarity.
Benefits of Indirect Ophthalmoscopy:
Indirect ophthalmoscopy offers several distinct advantages over direct ophthalmoscopy, making it the preferred technique for more comprehensive eye examinations. Here are some of its key benefits:
- Wider Field of View: One of the primary benefits of indirect ophthalmoscopy is its ability to provide a much wider field of view compared to direct ophthalmoscopy. The examiner can assess the peripheral retina, which is difficult to examine using the direct method. This is particularly important for detecting conditions like retinal detachments, diabetic retinopathy, and peripheral retinal tears that may not be visible with direct ophthalmoscopy.
- Three-Dimensional Visualization: The three-dimensional nature of indirect ophthalmoscopy gives the examiner a more realistic and comprehensive view of the retinal structures. This makes it easier to identify issues such as retinal folds, macular edema, or optic nerve head abnormalities.
- Enhanced Magnification: The combination of the lens and light source used in indirect ophthalmoscopy allows for greater magnification of the retina and optic nerve. This can aid in identifying subtle changes in the eye’s structures, which may not be detectable with direct ophthalmoscopy.
- Better for Eye Conditions Requiring Close Monitoring: Indirect ophthalmoscopy is particularly useful for patients with conditions like diabetic retinopathy, glaucoma, and retinal detachment. The technique allows for better monitoring of disease progression and the early detection of complications that could affect the patient’s vision.
- Greater Comfort for Patients: Indirect ophthalmoscopy can be less intrusive for patients than direct ophthalmoscopy, as the examiner does not need to be as close to the eye. This may help reduce patient discomfort, especially for those with light sensitivity or difficulty holding their eyes open.
Conclusion:
Indirect ophthalmoscopy is a highly effective and essential tool for diagnosing and managing various ocular conditions. By providing a wider and more detailed view of the retina and optic nerve, it allows eye care professionals to detect potential issues that could lead to vision loss. For an accurate examination using indirect ophthalmoscopy, it’s important to choose a well-equipped and specialised Eye Hospital, such as Infigo, where advanced technology and expert care come together to ensure the best possible outcomes for your eye health.